Nurse Staffing
Our health care system faces immense challenges. Cost-cutting decisions, an aging population, increased patient complexity and need, and an aging workforce all contribute to the current nurse staffing crisis that is negatively affecting nurses’ mental health and well-being.
Evidence shows appropriate nurse staffing contributes to improved patient outcomes and greater satisfaction for both patients and nurses. Addressing nurse staffing challenges supports our nurses, our patients, and our nation’s health and well-being.
Minimum nurse-to-patient ratios is one of many alternatives and solutions to achieve appropriate nurse staffing. The American Nurses Association (ANA) supports enforceable ratios as an essential approach to achieving appropriate nurse staffing.
Long-standing nurse staffing challenges will require multiple strategies. When considered together, they will improve the work environment and the ability of nurses to consistently provide safe patient care.
Appropriate nurse staffing is achievable, and the ANA supports all nurses in advocating for the staffing solutions they find most suitable in their practice settings. Read on to find out more about how ANA is working to improve nurse staffing and how you can get involved.
In This Section
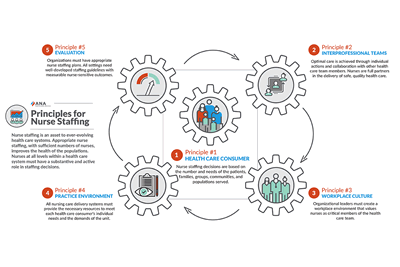
ANA Position Statements & Principles
Legislation & Regulation
Identifying and maintaining the appropriate nurse staff numbers and mix is critical to the delivery of quality patient care. Numerous studies reveal an association between higher levels of experienced RN staffing and lower rates of adverse patient outcomes.
When health care employers fail to recognize the association between RN staffing and patient outcomes, laws and regulations become necessary.