Jen Bonamer
PhD, RN, AHN-BC, NPD-BC
Nursing Professional Development – Research Specialist
Education, Professional Development & Research Department
Sarasota Memorial Health Care System
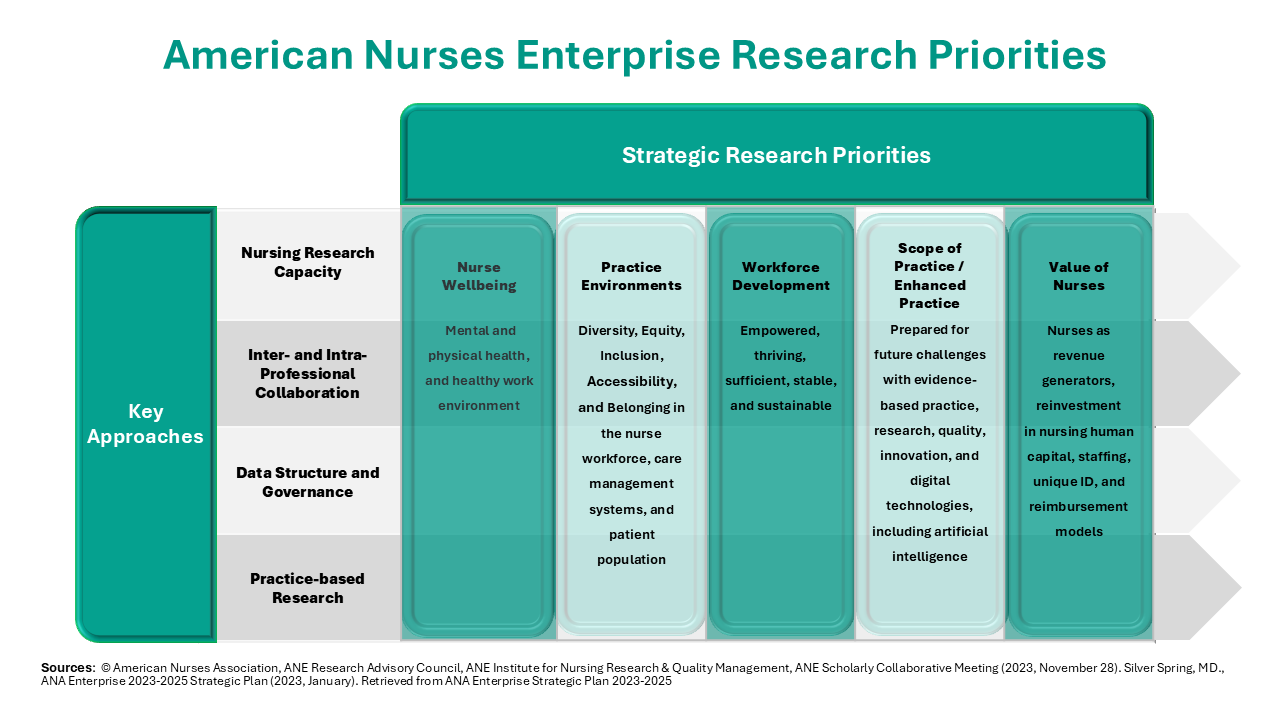
Jen Bonamer works as a Nursing Professional Development – Research Specialist at Sarasota Memorial Hospital in Sarasota, Florida. She leads the nursing research and evidence-based practice programs and is actively focused on supporting healthy work environments and clinician well-being. Jen received her BSN from the University of Florida (Gainesville) and practiced for ten years in pediatrics (general practice and hematology/oncology/bone marrow transplant). She completed the University of South Florida’s (Tampa) Nursing BS to PhD program with her master’s of science degree (nursing education) and PhD (nursing). She is certified in both nursing professional development and advanced holistic nursing. Jen is an active member in the American Nurses Association – Enterprise (ANAE) Research Advisory Council and an independent contractor of peer review services for the Magnet program.