Infection Control and Prevention
Infection control measures are important in the prevention and mitigation of COVID-19 spread within health care facilities. For guidelines on preparedness, infection control, and personal protective equipment (PPE) use and supply optimization, we have compiled a comprehensive list of resources for you to access.
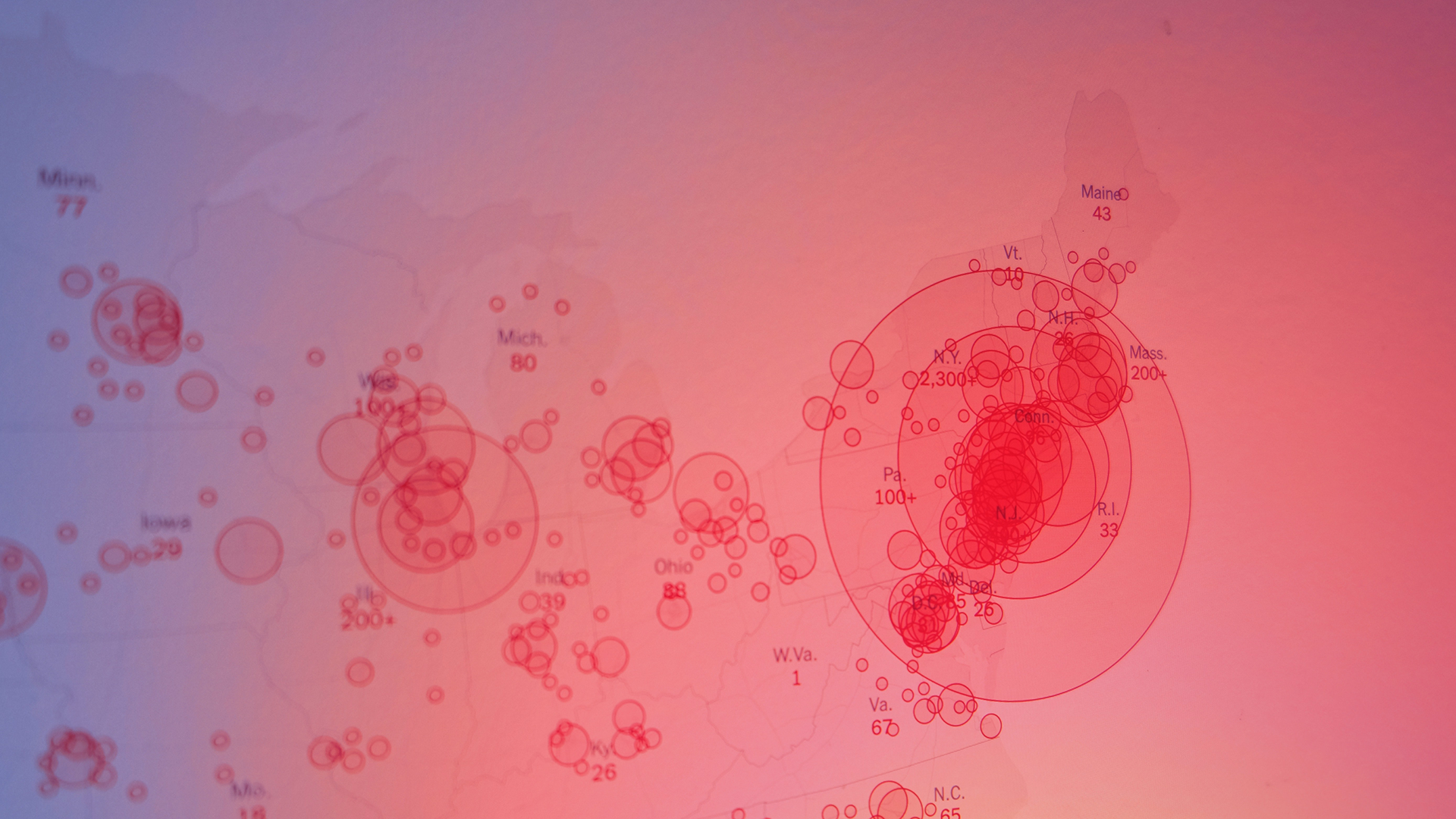
It’s also important to know and understanding how COVID-19 is spreading within your local community. To access your local health department for updated data, click on the map found here to access your County and City Health Officials.
Infection Control
- Infection Control Basics
Learn the basics of infection control to stop the spread of infection within your health care setting.
- Standard Precautions
Learn the basics about measures used for all patients to prevent the spread of infection within a health care facility and amongst staff and patients.
- Transmission-Based Precautions (Guidelines for contact, droplet, and airborne precautions)
Used in conjunction with standard precautions, learn about the different infection control measures based upon type of infection and route of transmission.
- Some COVID-19 patients can manage their symptoms from home. Find information to provide to your patients about caring for COVID-19 symptoms from home and reducing community spread of the virus.
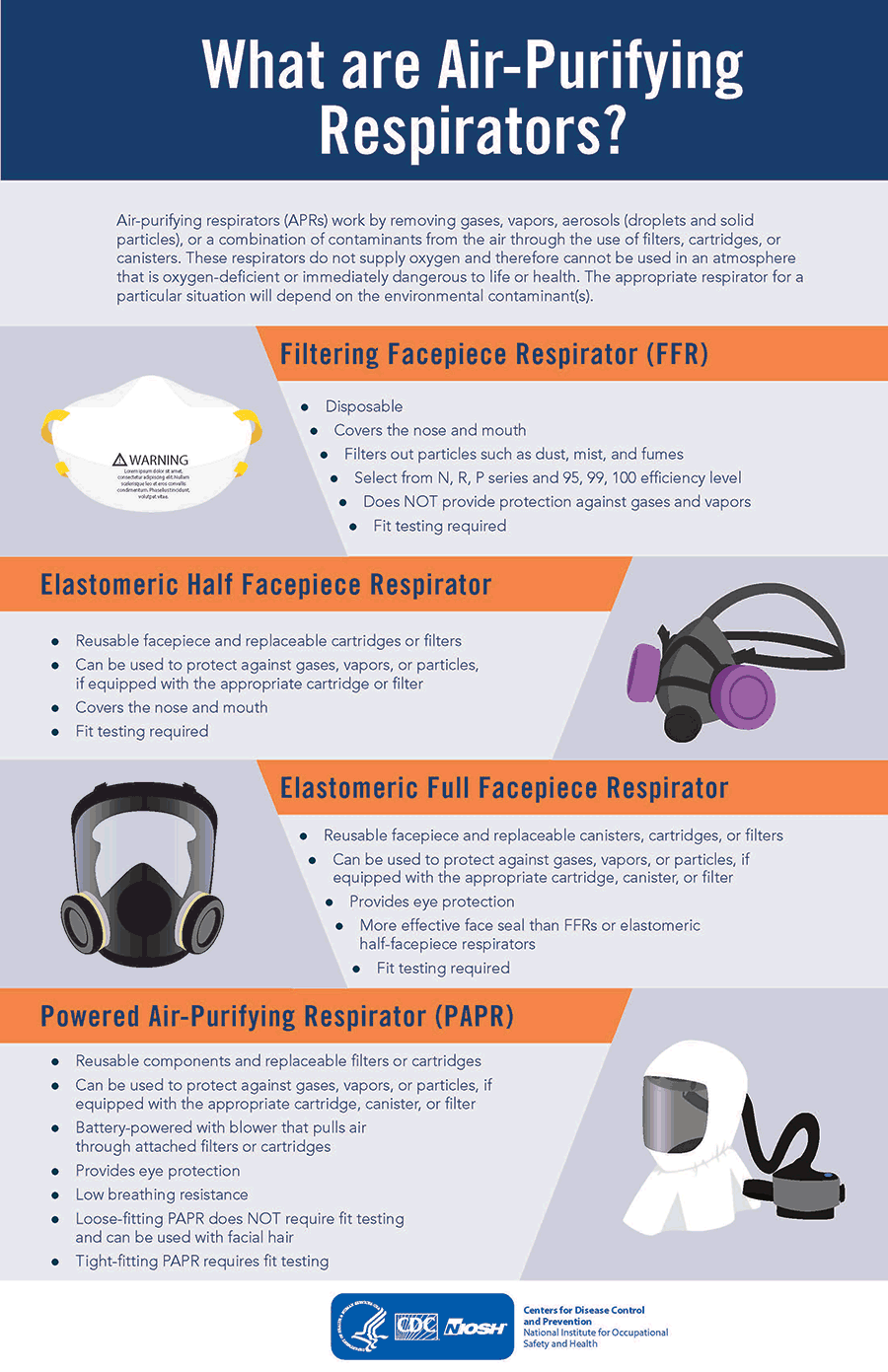
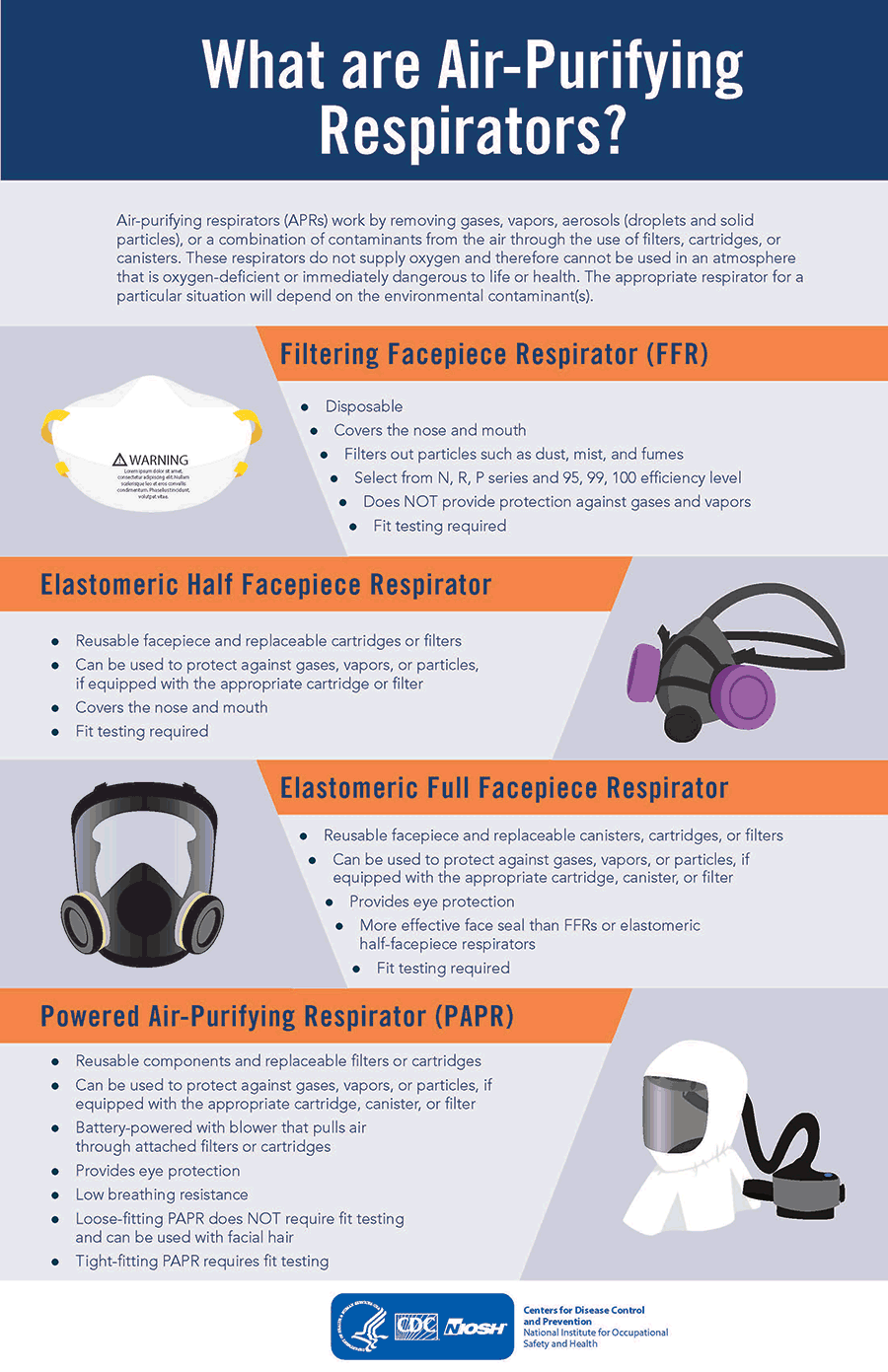
Personal Protective Equipment (PPE)
- Three Key Factors Required for a Respirator to be Effective
Whether you are using a newly issued N95 respirator or testing your N95 following extended use or reuse, these steps will help you ensure proper fit. If you are using a re-issued N95 that has been decontaminated, visually inspect if for cleanliness, check the straps for elasticity, and perform a seal check prior to performing patient care. If administering aerosolizing procedures, ask for a brand new N95 respirator.
- Safe Alternatives for Respirator Reuse
Half-Mask Elastomeric Respirators and Powered Air Purified Respirators (PAPR) are respirators intended for decontamination and reuse.