The ANA Enterprise is committed to informing and supporting nurses during the coronavirus (COVID-19) pandemic.
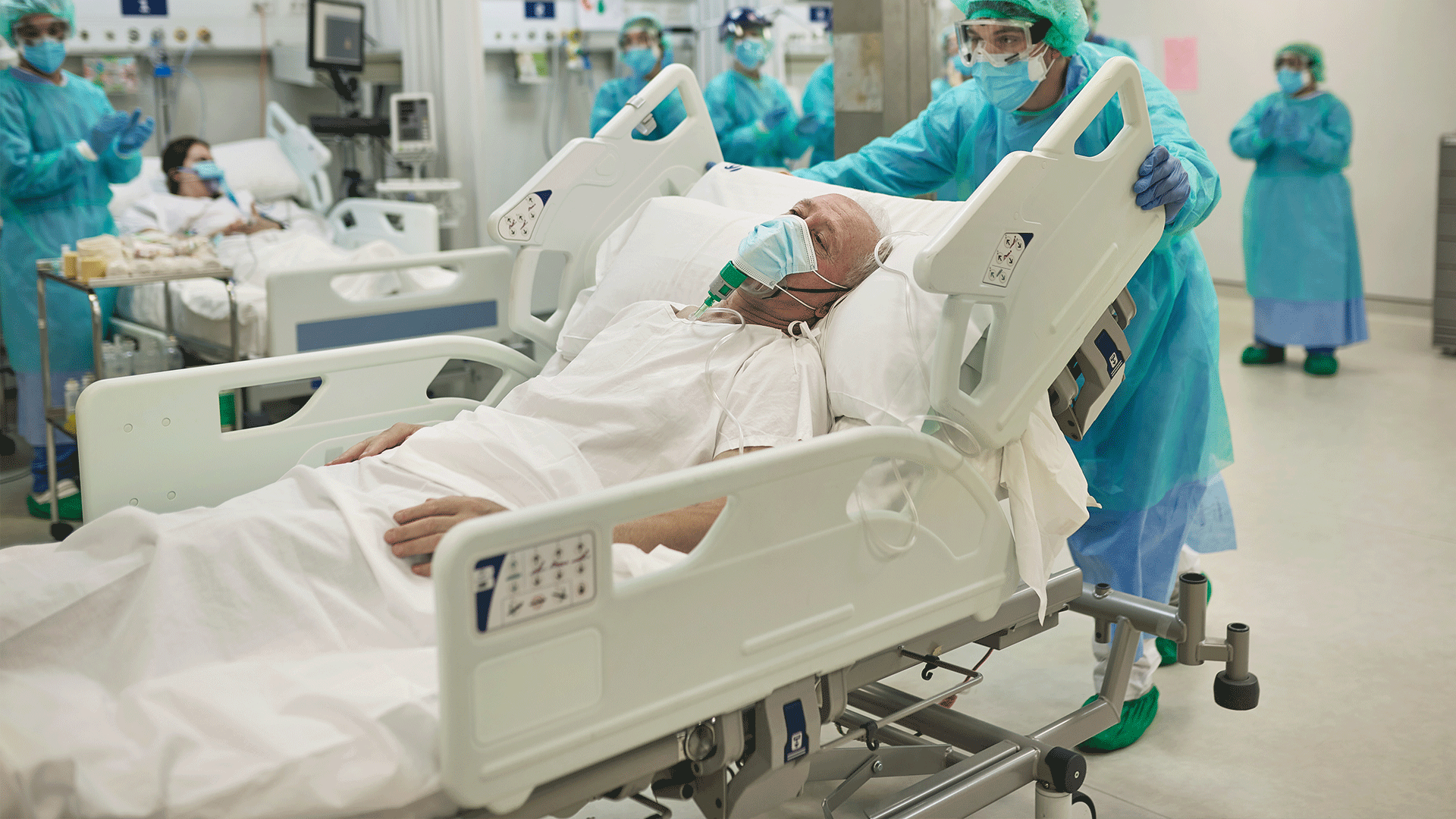
Read MoreIn the midst of the pandemic, nurses were called upon and put years of education and training into action. When everyone else ran from the storm, nurses ran directly into the middle of it all.
In these extraordinary times, the American Nurses Association is here for all nurses, because our life’s work is supporting your life’s work.

Sign up today for the latest information, new resources, and valuable tools from ANA COVID-19 Resource Center.
Learn More